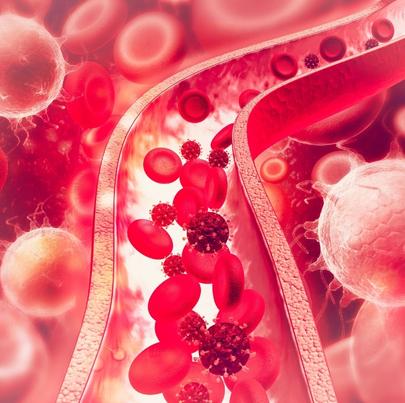
Bloodstream infections in hospital patients are a growing concern. According to the CDC, hospital-acquired infections are a major cause of death to patients, especially those that involve the bloodstream or lungs.
Hospital-Acquired Bloodstream Infections
Hospital-acquired infections are caused by fungal, viral and bacterial pathogens. The most common types are bloodstream infections, pneumonia and lung infections, urinary tract infections, and surgical site infections. Bloodstream infections, often called blood poisoning, are extremely dangerous, because bacteria and toxins can be carried to any part of the body through the bloodstream. Hospital-acquired bloodstream infections are a leading cause of injuries and fatalities seen by a personal injury lawyer. Based on data from death certificates, hospital acquired bloodstream infections are the 10th leading cause of death in the United States with an estimated 250,000 cases each year.
The Centers for Disease Control (CDC) recently conducted clinical studies in 49 different hospitals throughout the United States. Findings show that 51% of hospital-acquired bloodstream infections occur in intensive care units, 38% in internal medicine units, 20% in surgical units, and 13.5% in pediatric wards. Intravascular devices such as central venous catheters, intravenous catheters, arterial catheters, and urinary catheters showed the highest potential risk for patient bloodstream infections.
Bloodstream infections occur in both adult and pediatric patients. Among adults, there is no defined age group, but 45% of adult victims are women. In pediatric patients, babies with an extremely low birth weight, children younger than one year of age, and children in the neonatal intensive care unit or pediatric intensive care unit have higher rates of hospital-acquired bloodstream infections.
Central-Line Infections
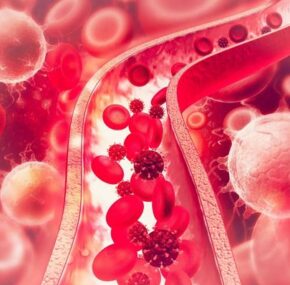
In hospitals, bloodstream infections commonly occur when germs multiply on a central-line device and enter the bloodstream. A central line is a catheter that’s inserted into a large vein, usually in the chest, neck, arms or groin area. It is typically used to draw blood or give patients who are critically ill medications and fluids. If necessary, a central line can be left in place for several weeks or months. These types of infections are very dangerous for patients because they can spread quickly to different internal organs, causing severe injuries and death.
The CDC estimates that there are 41,000 bloodstream infections caused by contaminated central lines in U.S. hospitals every year. To prevent central-line infections, they recommend that healthcare workers follow guidelines for sterile central line insertions and remove central lines from patients as soon as they are no longer needed.