Bedsore life expectancy depends on the patient’s prior condition, the speed of treatment received, and other health risks. Bedsores are a common sign of nursing home neglect, and family members should take quick action once their presence is discovered. They occur when there is unrelieved pressure on the skin and can lead to serious, potentially life-threatening infections.

(Article continues below infographic)
The Prevalence of Bedsores
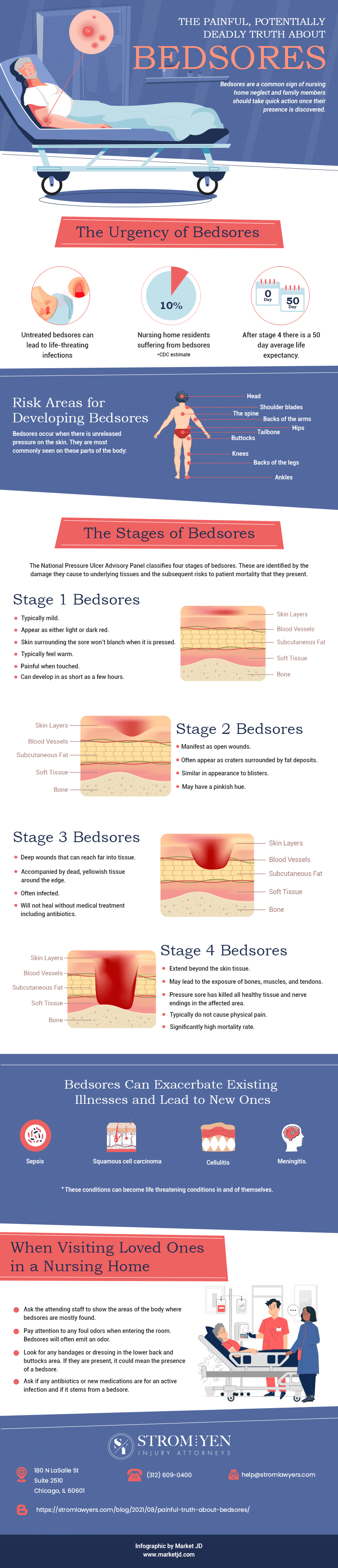
The CDC estimates that as many as 10% of nursing home residents suffer from bedsores. It is far from a new problem, and the prevalence of bedsores in nursing homes has been recognized for decades. Studies conducted by the National Pressure Ulcer Advisory Panel, CDC, and other entities have drawn a direct correlation between the presence of bedsores and patient mortality. The more advanced the bedsore, the greater the possibility that the nursing home resident will pass away from the injury. By some accounts, patients with Stage 4 bedsores have an average life expectancy of just 50 days once the condition has progressed to that level of severity.
Risk Factors for Developing Bedsores
While every nursing home resident is at risk for developing bedsores, there are some that are at greater risk than others. Individuals who are dependent upon wheelchairs and individuals who are confined to bed for long periods of time are at greatest risk. Pressure sores can be caused by friction between the skin and clothing or bedding, shears that occur when skin tissue is pulled in an opposite direction from bone structures, or sustained pressure that occurs when a nursing home resident’s body is immobile for an extended period of time.
Bedsores can be found on all areas of the body. However, they are most commonly seen on the buttocks, tailbone, backs of the arms and legs, the spine, shoulder blades, head, knees, ankles, and hips. This is because these areas are typically those that the weight of an individual’s body will rest upon while laying or sitting.
Bedsore Stages
The NPUAP classifies four bedsore stages. These are identified by the damage they cause to underlying tissues and the subsequent risks to patient mortality that they present. Bedsores can develop quickly and will progress at varying rates depending on the patient’s overall health and whether prompt treatment is provided.
The majority of patients with Stage 1 or Stage 2 bedsores can recover within a period of 2-3 weeks when prompt treatment is applied. However, the prognosis worsens for those with Stage 3 or 4 bedsores. Of those with Stage 4 bedsores, mortality rates can climb up to 70% within 180 days of onset.
Stage 1 Bedsores – These bedsores are typically mild and will appear as either light or dark red depending on the individual’s skin tone. They are identified because the skin surrounding the sore won’t blanch when it is pressed. These sores typically feel warm and will cause pain when touched. Stage 1 bedsores can develop quickly, sometimes as short as a few hours.
Stage 2 Bedsores – Stage 2 bedsores manifest as open wounds. These often appear as craters that are often surrounded by fat deposits around their edges. Often, these sores are similar in appearance to blisters and may have a pinkish hue.
Stage 3 Bedsores – These are deep wounds that can reach far into tissue. They are often accompanied by dead, yellowish tissue around the edge of the sore. These sores are often infected and will not heal without the application of medical treatment, including antibiotics.
Stage 4 Bedsores – Stage 1-3 bedsores that are not treated can quickly become Stage 4 bedsores. These sores extend beyond the skin tissue and may lead to the exposure of bones, muscles, and tendons. These sores typically do not cause physical pain because, by the time the pressure sore has reached this stage, it has killed all healthy tissue and nerve endings in the affected area. Stage 4 bedsore life expectancy is lower, and these deeper sores have a significantly high mortality rate.
Bedsore Life Expectancy and Related Illnesses
Bedsores often cause infections such as sepsis that can quickly spread throughout the bloodstream. They can also lead to the development of squamous cell carcinoma, cellulitis, and meningitis. These conditions can not only complicate the treatment of other existing conditions and have a serious impact on the individual’s quality of life, but they can also become life-threatening conditions in and of themselves.
Liability for Bedsores
Nursing home providers are responsible for the nursing home neglect that occurs within their facility. Staff, managers, and owners can be held liable for the personal injuries, medical expenses, impact on quality of life, and pain and suffering of the patients under their care. Moreover, they may be held liable should a pressure sore lead to the untimely death of the patient such as through infection, the development of cancer, etc. A nursing home neglect lawyer can help prepare documentation including photographs, witness statements, and medical records that establish the development and progression of the bedsores.
What to Look For
When visiting a relative at the nursing home, loved ones should be sure to ask the attending staff to show them the areas of the body where bedsores are mostly found. Visitors can also pay attention to any foul odors when entering the room. Bedsores will often emit an odor.
It is also a good idea to look for any bandages or dressing in the lower back and buttocks area. If they are present, it could mean the presence of a bedsore.
If a relative is unexpectedly on a regimen of antibiotics, family members might also ask if the medication is for an active infection and if it stems from a bedsore.








